Follow Your Passion: A Seamless Tumblr Journey
Pharmacy Technician - Blog Posts
How to Write a Case Study

The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics

In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression

Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
10 Simple Tips for Caring for Your Heart.

The heart, a tireless worker at the core of our well-being, demands our attention and care. As we navigate through Heart Health Month this February, let’s explore ten simple yet impactful tips to ensure our hearts thrive. These practices, ranging from physical activity to laughter and dental hygiene, collectively contribute to a holistic approach to cardiovascular wellness.
1.Cardiovascular Exercise: A Heart’s Best Friend
Engaging in regular cardiovascular or aerobic activities is fundamental for heart health. Following the American Heart Association’s recommendations of 75 minutes of vigorous exercise or 150 minutes of moderate-intensity exercise weekly can significantly boost cardiorespiratory fitness. Activities such as running, cycling, or brisk walking not only elevate heart rate but also enhance overall cardiovascular function. The rhythmic contraction and relaxation of muscles during exercise contribute to improved blood flow and reduced strain on the heart.
2.Embrace a Smoke-Free Lifestyle
Quitting smoking is a paramount step in safeguarding your heart. Smoking damages both the heart and blood vessels, escalating the risk of cardiovascular diseases. Additionally, avoiding second-hand smoke is crucial, as it has been linked to heart attacks and strokes. The harmful chemicals in tobacco smoke lead to the narrowing of blood vessels, increasing the workload on the heart and elevating the risk of high blood pressure.
3.Prioritize Quality Sleep
Adequate sleep, often underestimated, plays a pivotal role in heart health. With at least seven hours of nightly rest, blood pressure lowers, and the body undergoes essential repair processes. Research underscores the correlation between poor sleep and heightened risks of high blood pressure, subsequently increasing the likelihood of heart diseases. Establishing a consistent sleep routine and creating a conducive sleep environment are crucial steps in promoting optimal cardiovascular health.
4.Regular Checkups: A Heart-Healthy Habit
Consistent visits to the doctor for heart health checkups are essential. Assessing risk factors such as diet, blood pressure, cholesterol, and family history enables early detection and management of potential issues. A proactive approach to heart health empowers individuals to make informed lifestyle choices. Regular checkups also provide an opportunity for healthcare professionals to offer personalized guidance on maintaining heart health through tailored interventions.
5.Laughter: The Heart’s Natural Tonic
Laughing, whether through entertainment or social interactions, yields surprising benefits for the heart. The act of laughter reduces artery inflammation, lowers stress hormones, and increases levels of good cholesterol. Integrating humor into daily life becomes a delightful prescription for heart health. Laughter promotes the release of endorphins, the body’s natural feel-good chemicals, which contribute to overall well-being and stress reduction.
6.Dental Hygiene and Heart Connection
Surprising as it may seem, maintaining good dental hygiene contributes to heart health. Studies reveal a link between poor dental health and the presence of bacteria in the bloodstream, impacting heart valves. Simple practices such as regular brushing can significantly decrease the risk of cardiovascular disease. Furthermore, regular dental checkups not only preserve oral health but also serve as a preventive measure against potential cardiovascular complications.
7.Fuel Your Heart with a Healthy Diet
A heart-healthy diet rich in fruits, whole grains, vegetables, and legumes significantly improves blood pressure and cholesterol levels. Steering clear of salty foods and saturated fats is crucial, as they contribute to elevated blood pressure and increased bad cholesterol. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, further supports heart health by reducing inflammation and promoting optimal functioning of blood vessels.
8.Maintaining a Healthy Weight: A Heart’s Delight
Striving for and maintaining a healthy weight is a powerful defense against heart disease and high blood pressure. A combination of a balanced diet, regular exercise, and mindful calorie intake promotes overall well-being and cardiovascular health. Excess weight puts additional strain on the heart, leading to conditions such as hypertension and diabetes. Adopting sustainable lifestyle changes, including portion control and regular physical activity, contributes to achieving and sustaining a healthy weight.
9.Hydration: The Heart’s Elixir
Staying adequately hydrated is a simple yet often overlooked aspect of heart care. Considering the heart’s continuous effort in pumping around 2,000 gallons of blood daily, increased water intake supports its optimal functioning. Dehydration can lead to thicker blood, making the heart work harder to pump blood through the vessels. Maintaining proper hydration levels ensures the efficient transport of nutrients and oxygen to cells, promoting overall cardiovascular health.
10.Stay Active, Break Inactivity
Combatting sedentary lifestyles is crucial in preserving heart health. Incorporating simple changes like taking the stairs, walking, playing with pets, or engaging in household chores helps keep the heart active, reducing the risk of cardiovascular diseases. Prolonged sitting has been associated with various health risks, including obesity and heart disease. Regular physical activity not only supports cardiovascular health but also contributes to weight management and overall well-being.
In conclusion, adopting these ten heart-healthy habits provides a comprehensive approach to cardiovascular wellness. Whether it’s the joyous act of laughter, the discipline of regular exercise, or the mindfulness of a balanced diet, each step contributes to the harmonious symphony of a healthy heart. As we celebrate Heart Health Month, let’s embrace these practices and gift our hearts the care they deserve. Through consistent efforts and lifestyle modifications, we can ensure that our hearts continue to beat with vitality and resilience.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
Interesting Nursing Topics To Choose For A Case Study

Childhood Nursing
Antibiotics Impact on Childhood Immunities
Antibiotics have revolutionized modern medicine, significantly improving the prognosis for many infectious diseases. However, the impact of antibiotics on childhood immunities is a multifaceted topic that warrants careful examination. While antibiotics target harmful bacteria, they may also affect the delicate balance of the immune system in developing children.
Research could delve into the long-term consequences of antibiotic use during childhood, exploring how it may influence the development of the immune system. Are there specific types of antibiotics that pose greater risks? What role do probiotics play in mitigating the potential negative effects of antibiotics on the immune system? Understanding these dynamics is crucial for optimizing pediatric care and ensuring the long-term health of children.
Effects of Childhood Exposure to Environmental Pollutants

Children are particularly vulnerable to environmental pollutants, and exposure during early life stages can have lasting health implications. Research in this area could focus on specific pollutants, such as air pollutants, heavy metals, or endocrine disruptors, and their impact on children’s health.
Exploring the effects of second-hand smoke inhalation during early life stages is particularly relevant. What are the respiratory and cardiovascular consequences of childhood exposure to second-hand smoke? How does environmental pollution contribute to respiratory conditions in children, and what preventive measures can be implemented?
Ethics of Pediatric Care
The ethical dimensions of pediatric care are intricate, involving considerations of autonomy, beneficence, and justice. Topics within this realm could include ethical dilemmas faced by pediatric nurses, such as decision-making in cases where parental and child interests may conflict.
Research may also explore the ethical implications of emerging technologies in pediatric care. For instance, what are the ethical considerations surrounding genetic testing in children? How can nurses navigate the ethical challenges posed by advances in pediatric treatments and interventions?
Genetic Factors of Diabetes in Children

The increasing prevalence of diabetes in children raises questions about the genetic factors contributing to this trend. Research in this area could delve into the genetic markers associated with pediatric diabetes, exploring the hereditary aspects of the disease.
Understanding the interplay between genetic predisposition and environmental factors is crucial. What role do lifestyle factors play in the manifestation of diabetes in genetically predisposed children? How can nurses incorporate genetic counseling into pediatric diabetes management to empower families with the knowledge needed for preventive strategies?
How Health in Children Can Affect Their Health Later in Life
The concept that early life experiences can shape health outcomes in adulthood is a key area of interest. Research could investigate the link between childhood health and long-term health trajectories. Are there specific childhood health indicators that serve as predictors of adult health issues?
Exploring the mechanisms through which childhood health influences adulthood health can guide nursing interventions. How can nurses promote healthy behaviors in children that have lasting effects on their well-being? What preventive measures can be implemented during childhood to mitigate the risk of chronic diseases in adulthood?
Adult Nursing
Analyzing the Benefits of Collaborative Nursing
Collaborative nursing involves interdisciplinary teamwork to enhance patient care outcomes. Research in this area could explore the benefits of collaborative nursing practices in diverse healthcare settings. What are the positive outcomes associated with collaborative care, such as improved patient satisfaction, reduced hospital readmissions, or enhanced treatment adherence?
Understanding the factors that contribute to successful collaboration is essential. How do effective communication and shared decision-making impact collaborative nursing efforts? What challenges do nurses face in interprofessional collaboration, and how can these challenges be addressed to optimize patient care?
Analyzing the Causes of Depression

Depression is a prevalent mental health concern affecting a significant portion of the adult population. Research into the causes of depression can provide valuable insights into preventive measures and targeted interventions. This could involve exploring the interplay between genetic, environmental, and psychological factors in the development of depression.
Investigating the role of adverse childhood experiences in predisposing individuals to depression in adulthood is a pertinent avenue. How can nurses identify individuals at risk based on early life experiences? What interventions can be implemented to break the cycle of depression rooted in childhood trauma?
Ethics of Data Collection in Adult Health Care
The ethical considerations surrounding data collection in adult health care are paramount, especially in the era of electronic health records and data-driven healthcare. Research could delve into the ethical challenges nurses face in collecting, storing, and utilizing patient data.
Exploring the perspectives of patients regarding data privacy and consent is crucial. How do patients perceive the use of their health data for research purposes? What safeguards can be implemented to ensure ethical data practices in adult health care settings?
Evolution of Nursing in a Specific Time Period
The evolution of nursing over time reflects changes in healthcare practices, societal attitudes, and technological advancements. Research in this area could focus on a specific time period, examining how nursing roles, responsibilities, and education have transformed.
For example, a study could explore the evolution of nursing during a period of significant healthcare reform. What were the key drivers of change, and how did nurses adapt to new models of care? Understanding historical contexts can inform current nursing practices and guide future developments in the profession.
Nonchemical Treatments for Bipolar Disorders

Bipolar disorders present unique challenges in terms of management and treatment. Research into nonchemical treatments for bipolar disorders can provide valuable alternatives or complementary approaches to medication-based interventions.
Exploring the efficacy of psychotherapy, cognitive-behavioral interventions, and lifestyle modifications in managing bipolar disorders is essential. How can nurses incorporate nonchemical treatments into holistic care plans for individuals with bipolar disorders? What role does patient education play in promoting self-management strategies for bipolar conditions?
Midwifery Nursing
Analysis of Caseload and Quality of Care for Underrepresented Groups
Midwives play a crucial role in maternal and infant care, yet disparities in care outcomes persist among underrepresented groups. Research in this area could investigate the caseloads and quality of care provided to women from marginalized communities.
Examining the experiences of midwives in catering to diverse caseloads can provide insights into challenges and opportunities. How do midwives adapt their care approaches to address the unique needs of underrepresented populations? What strategies can be implemented to ensure equitable access to high-quality midwifery care?
Analysis of Childbirth Experiences of Women with Autism

Pregnancy and childbirth can pose unique challenges for women with autism spectrum disorders. Research could explore the childbirth experiences of women with autism, considering factors such as sensory sensitivities, communication preferences, and support needs.
Understanding the specific needs of this population can inform midwifery practices and improve the overall childbirth experience. What adjustments can be made in maternity care settings to accommodate the needs of women with autism? How can midwives collaborate with other healthcare professionals to provide holistic care for pregnant individuals with autism?
Nonchemical Pain Management in Labor
Labor pain is a central aspect of childbirth, and nonchemical pain management approaches are gaining attention. Research in this area could focus on the effectiveness of non-pharmacological pain management methods during labor.
Exploring techniques such as hydrotherapy, massage, acupuncture, and mindfulness can provide valuable insights. How do these nonchemical methods influence pain perception and labor outcomes? What role can midwives play in promoting and facilitating the use of non-pharmacological pain management strategies during childbirth?
Role of Midwifery in Emergency Care
While childbirth is often a natural process, emergencies can arise, requiring swift and effective interventions. Research could investigate the role of midwives in emergency care.
Conclusion
In this expansive discussion, we have explored a variety of nursing research topics across different specializations. Each topic presents unique challenges, opportunities, and areas for further exploration within the field of nursing. Whether focusing on pediatric care, mental health, women’s health, or health care management, the diverse range of topics reflects the major areas to consider.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: expertassignment46@gmail.com for professional guidance.
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
Gangrene

Introduction
Gangrene, a condition marked by tissue death due to insufficient blood flow or bacterial infection, poses significant risks to affected individuals. Understanding the complexities surrounding gangrene, including its symptoms, causes, diagnosis, treatment modalities, and preventive measures, is paramount for healthcare professionals and the general public alike. This comprehensive discussion aims into the aspects of gangrene, providing insights into its various dimensions and fostering awareness for timely intervention and improved patient outcomes.
Overview of Gangrene
Gangrene manifests when tissues are deprived of adequate blood supply, leading to necrosis or cell death. Whether triggered by compromised circulation or bacterial invasion, gangrene can affect diverse anatomical regions, from the extremities to internal organs. Diabetes, atherosclerosis, and other vascular disorders heighten susceptibility to gangrene, underscoring the importance of vascular health in mitigating its onset.
Symptoms of Gangrene

Recognizing the subtle yet ominous signs of gangrene is critical for timely intervention. Symptoms encompass a spectrum of manifestations, including changes in skin color, swelling, blister formation, intense pain followed by numbness, malodorous discharge, skin texture alterations, and coolness upon touch. Systemic indicators such as fever, tachycardia, and hypotension may herald severe infection or septic shock, necessitating urgent medical attention.
When to See a Doctor
Prompt medical evaluation is imperative upon the onset of persistent, unexplained pain coupled with skin discoloration, discharge, or trauma-related symptoms. Delayed intervention can exacerbate tissue damage and precipitate life-threatening complications, underscoring the urgency of seeking professional care without delay.
Causes of Gangrene

Gangrene can arise from a constellation of etiological factors, ranging from vascular insufficiency to microbial infiltration. Conditions like diabetes, atherosclerosis, traumatic injury, or surgical interventions predispose individuals to gangrene by compromising tissue perfusion or facilitating pathogen colonization. Various subtypes of gangrene, including dry, wet, gas, internal, Fournier’s, and Maloney's gangrene, exhibit distinct pathophysiological mechanisms and clinical presentations, necessitating tailored therapeutic approaches.
Diagnosis and Treatment

Accurate diagnosis of gangrene entails a special evaluation of clinical symptoms, medical history, and ancillary investigations such as imaging and laboratory tests. Treatment strategies aim to restore tissue perfusion, eradicate infection, and remove necrotic tissue. Antibiotics, hyperbaric oxygen therapy, and surgical interventions like debridement or amputation constitute cornerstone modalities, guided by the severity and anatomical extent of gangrene.
Doctors and Departments
A multidisciplinary approach involving primary care physicians, vascular surgeons, infectious disease specialists, and wound care experts is indispensable for comprehensive management of gangrene. Collaborative efforts encompass diagnostic precision, therapeutic synergy, and rehabilitative support, ensuring holistic care tailored to individual patient needs.
Prevention
Preventing gangrene necessitates proactive measures targeting predisposing factors and promoting vascular health. Effective strategies encompass glycemic control in diabetes, lifestyle modifications, smoking cessation vigorous wound care, and early recognition of ischemic or infectious triggers. Vigilant surveillance and timely intervention mitigate the risk of gangrene development, fostering tissue preservation and optimizing long-term outcomes.
Conclusion
Gangrene epitomizes a formidable clinical challenge leading to various approach consisting of prevention, early recognition, and prompt intervention. Heightened awareness of gangrene’s clinical spectrum, coupled with proactive measures targeting predisposing factors, is important for mitigating its morbidity and mortality. By fostering collaboration among healthcare providers and empowering individuals with knowledge and preventive strategies, we can confront the scourge of gangrene and safeguard tissue viability, thereby promoting optimal health and well-being for all.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
The Endocrine System

Introduction
The endocrine system is a complex network containing a symphony of hormonal interactions crucial for maintaining physiological equilibrium. Comprising glands, organs, and tissues dispersed throughout the body, its influence allows various bodily functions, spanning from metabolism to reproduction and beyond. This topic endeavors to provide an in-depth exploration of the endocrine system, encompassing its anatomy, physiological functions, associated conditions, and strategies for proactive care. By indulging into this indispensable regulatory system, we aim to equip readers with a comprehensive understanding to prioritize their hormonal health effectively.
Anatomy of the Endocrine System
The anatomy of the endocrine system is contained by an array of specialized glands, organs, and tissues, each endowed with the capacity to synthesize and dispatch hormones into the bloodstream. Principal among these are:
Endocrine Glands: These specialized tissues, including the pituitary gland, thyroid gland, and adrenal glands, secrete hormones directly into circulation, exerting systemic effects.
Endocrine Organs: Organs such as the hypothalamus, pancreas, and reproductive glands contribute to hormonal regulation, interfacing closely with the nervous system to modulate physiological responses.
Endocrine-Related Tissues: Adjunct to traditional endocrine structures, adipose tissue, kidneys, and even the heart harbor the capability to produce hormones, further augmenting the system’s complexity and regulatory capacity.
Functions of the Endocrine System
The cardinal function of the endocrine system is hormone secretion, holding up varied network of intercellular communication. Hormones, acting as molecular messengers, traverse the bloodstream to target cells, eliciting diverse physiological responses.
Key functions include:
Metabolism Regulation: Hormonal content govern metabolic processes, dictating energy expenditure, glucose homeostasis, and lipid metabolism.
Homeostatic Control: Endocrine signaling regulates internal threshold, modulating blood pressure, fluid balance, and body temperature.
Development and Growth: Hormonal interplay underpins growth trajectories and developmental milestones, steering embryonic stages and pubertal maturation.
Sexual Function and Reproduction: Hormonal modulation governs reproductive physiology, controlling fertility, libido, and secondary sexual characteristics.
Neuroendocrine Integration: The endocrine system reveals intimately with the nervous system, harmonizing behavioral and physiological responses, including mood regulation and sleep-wake cycles.
Conditions and Disorders
A spectrum of endocrine-related ailments afflicts individuals, stemming from hormonal imbalances, glandular dysfunctions, or neoplastic proliferations. Noteworthy conditions encompass:
Diabetes and Metabolic Disorders: Spanning type 1 and type 2 diabetes, metabolic syndrome, and obesity, these conditions disrupt glucose homeostasis and metabolic equilibrium.
Endocrine Cancers and Tumors: Malignancies affecting endocrine tissues, including adrenal tumors, pituitary adenomas, and thyroid malignancies, necessitate specialized oncological management.
Thyroid Dysfunction: Hypo- and hyperthyroidism, thyroid nodules, and autoimmune thyroiditis typify prevalent thyroid disorders, precipitating diverse clinical manifestations.
Reproductive and Sexual Health Disorders: From polycystic ovary syndrome (PCOS) to erectile dysfunction, disruptions in reproductive hormone signaling manifest as infertility, menstrual irregularities, and sexual dysfunction.
Proactive Care and Health Maintenance
In fostering endocrine wellness, a holistic approach integrating lifestyle modifications and environmental awareness is imperative. Strategies for promoting endocrine health encompass:
Lifestyle Optimization: Embracing a balanced diet, regular exercise regimen, and adequate sleep hygiene fosters metabolic resilience and hormonal equilibrium.
Environmental Vigilance: Mitigating exposure to endocrine-disrupting chemicals pervasive in everyday products, such as plastics, pesticides, and personal care items, reduces the risk of hormonal perturbations.
Health Surveillance: Individuals with familial predispositions to endocrine disorders benefit from proactive screening and vigilant symptom monitoring, facilitating early intervention and optimal disease management.
Conclusion
The endocrine entails physiological regulation, producing hormonal interactions essential for vitality and well-being. By looking at anatomy, physiological functions, associated conditions, and avenues for proactive care, this discourse endeavors to foster a comprehensive understanding of the endocrine system Empowered with knowledge, individuals can prioritize their hormonal health, embracing proactive measures to optimize their overall well-being and quality of life.
For medical students navigating the study of endocrinology and seeking guidance and academic support during their study period, Expert Academic Assignment Help offers invaluable assistance. With our expertise and resources, we provide tailored solutions to aid in comprehension, research, and academic success. Don’t hesitate to reach out to us for personalized assistance and elevate your understanding of this vital field. Your academic journey awaits, and we’re here to help you excel.
Contact us at expertassignment46@gmail.com for professional assistance,
Pulmonary Edema

Introduction
Pulmonary edema is a condition that results from the abnormal accumulation of fluid in the lungs, leading to impaired gas exchange and respiratory distress. This comprehensive discourse aims to provide an in-depth analysis of pulmonary edema, covering its pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications.
Pathophysiology of Pulmonary Edema

Pulmonary edema develops when there is an imbalance between the hydrostatic and oncotic pressures within the pulmonary vasculature. This imbalance leads to an increase in capillary permeability and the extravasation of fluid into the interstitial space and alveoli of the lungs. Several mechanisms contribute to this process, including increased capillary hydrostatic pressure due to heart failure, increased vascular permeability due to inflammation or injury, and decreased oncotic pressure due to hypoalbuminemia or capillary leak syndrome.
Etiology of Pulmonary Edema
The etiology of pulmonary edema can be categorized into cardiogenic and noncardiogenic causes. Cardiogenic pulmonary edema occurs secondary to heart failure or other cardiac conditions that result in elevated left atrial pressure and pulmonary venous congestion. Noncardiogenic pulmonary edema, on the other hand, is caused by factors unrelated to heart dysfunction, such as acute respiratory distress syndrome (ARDS), aspiration, sepsis, or neurogenic pulmonary edema.
Clinical Manifestations of Pulmonary Edema

The clinical presentation of pulmonary edema varies depending on the underlying cause and severity of the condition. Common symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, frothy sputum, cyanosis, and crackles on auscultation. Severe cases may progress to respiratory failure, hypoxemia, and hemodynamic instability.
Diagnostic Modalities for Pulmonary Edema

Diagnosing pulmonary edema requires a thorough clinical evaluation, including a detailed medical history, physical examination, and various diagnostic tests. Imaging studies such as chest X-ray, computed tomography (CT) scan, and lung ultrasound can provide valuable information about lung parenchymal changes and the presence of pulmonary congestion. Laboratory tests, including arterial blood gas analysis, brain natriuretic peptide levels, and electrolyte measurements, may also aid in the diagnosis and assessment of disease severity.
Treatment Strategies for Pulmonary Edema
The management of pulmonary edema involves addressing the underlying cause, relieving symptoms, and preventing complications. Initial treatment often includes supplemental oxygen therapy to improve oxygenation and reduce respiratory distress. Diuretics, such as furosemide or bumetanide, are commonly used to reduce fluid overload and alleviate pulmonary congestion. In cases of cardiogenic pulmonary edema, vasodilators, inotropes, or mechanical ventilation may be necessary to improve cardiac function and gas exchange.
Prevention Strategies for Pulmonary Edema
Preventing pulmonary edema requires a broad approach aimed at managing underlying risk factors and promoting healthy lifestyle habits. Patients with known cardiac conditions should adhere to prescribed medications, maintain a low-sodium diet, and monitor fluid intake to prevent fluid retention and exacerbation of heart failure. Individuals at risk of noncardiogenic pulmonary edema should avoid exposure to toxins, practice proper respiratory hygiene, and seek prompt medical attention for respiratory infections or injuries.
Complications of Pulmonary Edema

Untreated or inadequately managed pulmonary edema can lead to several complications, including acute respiratory distress syndrome (ARDS), cardiogenic shock, acute kidney injury, pulmonary hypertension, and death. Prompt recognition and intervention are essential to prevent progression to these life-threatening complications and improve patient outcomes.
Conclusion
Pulmonary edema is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and appropriate management. By understanding the underlying pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications of pulmonary edema, healthcare providers can optimize patient care and outcomes. Continued research efforts aimed at elucidating the mechanisms underlying pulmonary edema and identifying novel therapeutic targets are essential to further improve patient outcomes and reduce the global burden of this condition.
Embarking on your journey in the field of medicine is both exciting and challenging. As you navigate through your rigorous study period, it’s essential to seek guidance and assistance whenever needed to ensure your success.
At Expert Academic Assignment Help, we understand the demands of medical education and are here to support you every step of the way. Whether you require assistance with assignments, research papers, or exam preparation, our team of experts is dedicated to providing you with the help you need to excel in your studies.
Don’t hesitate to reach out to us for guidance, academic support, or any questions you may have. You can contact us via email at expertassignment46@gmail.com
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
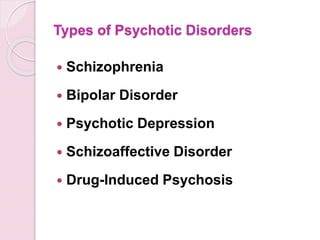
Types of Psychotic Disorders
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
Cirrhosis Of The Liver

Introduction
Cirrhosis stands as a challenge in the narrative of liver disease, marking the culmination of a complex interplay of factors that converge to undermine the organ’s structural integrity and functional capacity. This condition, characterized by the progressive accumulation of scar tissue within the liver parenchyma, holds a cascade of physiological network that reverberate throughout the body, manifesting in a spectrum of symptoms and complications. From its inner onset to its profound implications for morbidity and mortality, cirrhosis generate the intricate interplay between genetic predisposition, environmental influences, and individual behaviors.
In this comprehensive discussion, we embark on an exploration of the multifaceted dimensions of cirrhosis, traversing its etiological underpinnings, clinical manifestations, diagnostic modalities, therapeutic strategies, and avenues for prevention and self-care. By delving into the intricacies of cirrhosis, we endeavor to elucidate the imperative of early recognition, proactive intervention, and holistic management in ameliorating its adverse sequelae and fostering optimal outcomes for affected individuals
Pathophysiology of Cirrhosis

Central to the pathogenesis of cirrhosis lies a complex interplay of molecular and cellular events that precipitate the gradual transformation of healthy hepatic tissue into fibrotic scar tissue. At the heart of this process lies fibrogenesis, wherein a multitude of cellular players, including hepatic stellate cells, inflammatory mediators, and extracellular matrix proteins, triggers a profibrotic milieu in response to persistent liver injury and inflammation. The ensuing deposition of collagen-rich scar tissue disrupts the structure of the liver lobules, impeding normal hepatocellular function and vascular dynamics.
Symptoms and Clinical Manifestations

The clinical presentation of cirrhosis spans a broad spectrum, reflecting the diverse array of physiological derangements engendered by advanced liver disease. Early-stage cirrhosis may manifest subtly, with nonspecific symptoms such as fatigue, malaise, and vague abdominal discomfort, often eluding timely diagnosis. However, as the disease progresses, overt signs of hepatic decompensation emerge, including jaundice, ascites, hepatic encephalopathy, and gastrointestinal bleeding, heralding the onset of life-threatening complications. Moreover, cirrhosis exerts systemic effects beyond the confines of the liver, precipitating coagulopathy, renal dysfunction, and metabolic disturbances.
Etiology and Risk Factors
Cirrhosis arises from an influence of etiological insults, encompassing a diverse spectrum of predisposing factors that contribute to hepatocellular injury and fibrogenesis. Foremost among these is chronic alcohol abuse, which inflicts direct hepatotoxic effects and potentiates oxidative stress and inflammatory cascades within the liver microenvironment. Additionally, viral hepatitis infections, particularly hepatitis B and C, constitute major drivers of cirrhosis worldwide, underscoring the imperative of vaccination and antiviral therapy in disease prevention and management. Other contributing factors include nonalcoholic fatty liver disease, autoimmune disorders, hereditary hemochromatosis, and biliary tract diseases, each exerting a unique influence on cirrhosis pathogenesis.
Diagnostic Modalities

Accurate diagnosis forms the linchpin of effective cirrhosis management, necessitating a judicious amalgamation of clinical symptoms, laboratory investigations, imaging modalities, and histopathological evaluation. Liver function tests serve as indispensable tools for gauging the synthetic and metabolic capacity of the liver, while imaging studies such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) afford insights into hepatic morphology, vascular dynamics, and the presence of focal lesions. Despite their utility, these modalities may be supplemented by liver biopsy, which remains the gold standard for assessing the degree of fibrosis and guiding therapeutic decisions, albeit fraught with procedural risks and sampling variability.
Treatment Strategies

While cirrhosis represents a chronic and irreversible condition, therapeutic interventions are geared toward monitoring disease progression, alleviating symptoms, and forestalling the onset of complications. Pharmacological therapies, including hepatoprotective agents, antifibrotic agents, and symptom-based medications, aim to attenuate hepatic inflammation, inhibit fibrogenesis, and ameliorate symptom burden in cirrhotic patients. Furthermore, endoscopic interventions such as variceal band ligation and trans jugular intrahepatic portosystemic shunting play a major role in the management of portal hypertension and its sequelae, including variceal bleeding and refractory ascites. For select individuals with end-stage liver disease, liver transplantation offers a definitive therapeutic option, affording a second lease on life and circumventing the inexorable progression of cirrhosis-related complications.
Self-Care and Lifestyle

Empowering individuals with cirrhosis to adopt proactive self-care measures constitutes a cornerstone of comprehensive disease management, emphasizing the role of lifestyle modifications, dietary interventions, and preventive strategies in optimizing health outcomes. Lifestyle modifications, including abstinence from alcohol, adherence to a liver-friendly diet, regular exercise, and smoking cessation, are paramount in attenuating hepatic inflammation, promoting metabolic homeostasis, and mitigating cardiovascular risk factors in cirrhotic patients. Additionally, vaccination against hepatitis viruses, avoidance of hepatotoxic medications, and judicious monitoring of comorbid conditions serve as essential pillars of preventive care, safeguarding against disease exacerbations and fostering long-term wellness in individuals with cirrhosis.
Conclusion
Cirrhosis emerges as a complex and a dangerous disease, syndrome characterized by progressive hepatic fibrosis, compromised organ function, and a plethora of systemic manifestations. The etiological heterogeneity of cirrhosis underscores the need for a personalized and multidisciplinary approach to disease management, Focusing to the unique pathophysiological mechanisms and clinical manifestations inherent to each individual. Through timely diagnosis, targeted interventions, and collaborative care, healthcare providers can mitigate the burden of cirrhosis, optimize patient quality of life, and prolong survival in affected individuals. As we navigate complexities of cirrhosis, a concerted emphasis on preventive measures, patient education, and therapeutic innovations holds the key to unlocking a brighter prognosis for those afflicted by this formidable liver disease.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
Diabetes

Introduction to Diabetes
Diabetes, a metabolic disorder characterized by chronic hyperglycemia, arises from abnormalities in insulin secretion, insulin action, or both. The condition’s prevalence has reached epidemic proportions globally, with significant health, economic, and social implications.
Types of Diabetes

Type 1 Diabetes: This autoimmune disease results from the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Genetics and environmental triggers play pivotal roles in its pathogenesis. Despite being less common than Type 2 diabetes, its onset during childhood or adolescence significantly impacts individuals’ lives.
Type 2 Diabetes: Predominantly a disorder of insulin resistance, Type 2 diabetes accounts for the majority of diabetes cases worldwide. Lifestyle factors, genetic predisposition, and obesity contribute to its development. Its insidious onset often leads to delayed diagnosis and increased risk of complications.
Gestational Diabetes: Occurring during pregnancy, gestational diabetes poses risks to both maternal and fetal health. Hormonal changes and insulin resistance characterize its pathophysiology. Effective screening and management are crucial to prevent adverse outcomes.
Other Types of Diabetes: Variants like MODY, LADA, and secondary diabetes present unique challenges in diagnosis and management, requiring tailored approaches to care.
Epidemiology and Prevalence
Diabetes prevalence varies across demographics, with disparities observed in age, gender, ethnicity, and socioeconomic status. The escalating burden of diabetes underscores the urgent need for targeted prevention and management strategies.
Symptoms and Causes

Hyperglycemia-induced symptoms like polyuria, polydipsia, and unexplained weight loss serve as clinical indicators for diabetes diagnosis. Understanding the complex interplay of genetic, environmental, and lifestyle factors elucidates the condition’s etiology.
Complications
Diabetes complications encompass a spectrum of microvascular and macrovascular disorders, significantly impacting quality of life and life expectancy. From diabetic retinopathy to cardiovascular disease, nephropathy, neuropathy, and diabetic foot complications, the ripple effects of uncontrolled diabetes are profound.
Diagnosis and Tests

Accurate diagnosis relies on comprehensive evaluation, including fasting glucose, oral glucose tolerance tests, and hemoglobin A1c measurements. Screening recommendations aim to identify at-risk individuals early, facilitating timely intervention and risk reduction.
Management and Treatment
Diabetes management strategies encompass pharmacotherapy, lifestyle modifications, patient education, and multidisciplinary care. Individualized treatment plans address glycemic control, blood pressure management, lipid optimization, and prevention of complications.
Prevention
Prevention initiatives target modifiable risk factors through health promotion, public health interventions, and community engagement. Emphasizing the role of nutrition, physical activity, and behavioral changes empowers individuals to mitigate their diabetes risk.
Outlook and Prognosis
Prognostic factors such as glycemic control, adherence to therapy, comorbidity burden, and psychosocial support influence long-term outcomes. Enhanced collaboration among healthcare providers, policymakers, and stakeholders is essential to improve diabetes prognosis globally.
Living With Diabetes

Coping with diabetes requires resilience, self-management skills, and social support networks. Empowering individuals through education, self-monitoring tools, and peer support enhances their capacity to navigate the challenges of daily diabetes management.
Impact on Individuals and Society
Diabetes exerts a profound socioeconomic burden, encompassing healthcare costs, productivity losses, and reduced quality of life. Addressing the psychosocial dimensions of diabetes care is integral to fostering holistic well-being and societal resilience.
Future Directions and Research

Advancements in diabetes research, including precision medicine, digital health technologies, and novel therapeutics, offer promising avenues for disease management and prevention. Collaborative research endeavors aim to translate scientific discoveries into tangible clinical benefits.
Conclusion
In conclusion, diabetes represents public health challenge necessitating a comprehensive, patient-centered approach. By fostering awareness, promoting early detection, and advancing evidence-based interventions, we can mitigate the impact of diabetes on individuals, families, and communities worldwide.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
How to Write a Case Study

Introduction
The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics
In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression
Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
H. pylori Infection

Introduction
Helicobacter pylori (H. pylori) infection is a significant global health concern, affecting a substantial portion of the world’s population. The discussion aims to provide an in-depth exploration of various aspects of H. pylori infection, including its prevalence, transmission, symptoms, diagnosis, treatment, complications, prevention strategies, and future research directions.
Prevalence and Transmission

H. pylori infection is widespread, with approximately two-thirds of the world’s population harboring the bacterium in their gastrointestinal tract. Various factors contribute to its prevalence, including socioeconomic status, living conditions, hygiene practices, and geographic location. The discussion indulges into the epidemiological trends of H. pylori infection across different populations and regions, highlighting disparities in prevalence rates and associated risk factors.
Transmission of H. pylori occurs primarily through interpersonal contact and ingestion of contaminated food or water. Saliva, fecal-oral transmission, and oral-oral transmission, including through kissing, are significant modes of spread. Poor sanitation and overcrowded living conditions facilitate the transmission of the bacterium, particularly in resource-limited settings. The discussion explores the mechanisms of H. pylori transmission and the implications for public health interventions aimed at reducing its spread.
Symptoms and Diagnosis

While many individuals with H. pylori infection remain asymptomatic, others experience a range of gastrointestinal symptoms, including stomach pain, bloating, nausea, and weight loss. The discussion elucidates the spectrum of clinical manifestations associated with H. pylori infection, emphasizing the importance of recognizing atypical presentations and considering differential diagnoses.
Diagnosing H. pylori infection presents several challenges due to the variability of symptoms and the limitations of available diagnostic tests. We critically evaluates the utility of different diagnostic modalities, including stool antigen tests, urea breath tests, and upper gastrointestinal endoscopy, in detecting H. pylori infection. It also examines the role of serological tests and molecular techniques in enhancing diagnostic accuracy and guiding clinical management decisions.
Treatment Options

The standard treatment regimens for H. pylori infection typically involve a combination of antibiotics and proton pump inhibitors (PPIs). However, rising rates of antibiotic resistance pose significant challenges to effective eradication therapy. It explores the mechanisms of antibiotic resistance in H. pylori and the implications for treatment outcomes.
Alternative treatment approaches, such as sequential therapy, concomitant therapy, and bismuth-based quadruple therapy, are also examined in the context of their efficacy and tolerability. Highlighting the importance of individualizing treatment regimens based on antibiotic susceptibility testing and patient-specific factors to optimize therapeutic outcomes.
Complications

Peptic ulcers are a common complication of H. pylori infection, resulting from the bacterium’s ability to disrupt the gastric mucosal barrier and induce inflammation. The discussion elucidates the pathophysiology of peptic ulcer formation and the factors contributing to ulcer recurrence and complications.
In addition to peptic ulcers, H. pylori infection is associated with an increased risk of more serious complications, such as gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. The discussion explores the molecular mechanisms underlying H. pylori-induced carcinogenesis and the strategies for early detection and management of gastric neoplasms.
Prevention

Preventive measures play a crucial role in reducing the burden of H. pylori infection and its associated complications. The discussion emphasizes the importance of promoting good hygiene practices, including handwashing and sanitation, to minimize the risk of transmission.
Furthermore, dietary factors may influence the risk of H. pylori infection and its clinical outcomes. The discussion evaluates the evidence regarding the impact of dietary habits, such as consumption of fruits, vegetables, and probiotics, on H. pylori colonization and disease progression. It also addresses the potential role of vaccination in preventing H. pylori infection and its complications, highlighting ongoing research efforts in vaccine development.
Research and Future Directions
Ongoing research efforts are focused on advancing our understanding of H. pylori pathogenesis, identifying novel therapeutic targets, and developing effective preventive strategies. The discussion highlights recent advancements in H. pylori research, including insights into bacterial virulence factors, host immune responses, and microbial interactions within the gastric microbiota.
Future directions in H. pylori research encompass a multidisciplinary approach, integrating molecular biology, epidemiology, immunology, and clinical medicine. The discussion outlines key areas for future investigation, such as the development of targeted antimicrobial agents, the role of host genetics in H. pylori susceptibility, and the impact of microbial dysbiosis on disease outcomes.
Conclusion
In conclusion, H. pylori infection remains a significant public health challenge, with implications for gastrointestinal health and disease worldwide. A comprehensive understanding of the epidemiology, pathogenesis, diagnosis, treatment, and prevention of H. pylori infection is essential for guiding clinical practice and informing public health policies. By addressing the complexities of H. pylori infection through interdisciplinary research and collaborative efforts, we can strive towards reducing its global burden and improving patient outcomes.
In managing H. pylori infection, compassion, empathy, and a holistic approach are crucial alongside clinical expertise. Striving for excellence in knowledge and practice enables us to advance gastroenterology and improve patient outcomes.
As we address H. pylori infection and its broader implications on gastrointestinal health, let’s remain dedicated to providing optimal patient care. By working collaboratively and embracing interdisciplinary approaches, we can positively impact lives and contribute to a healthier future.
Email expertassignment46@gmail.com to explore how we can assist you in achieving your academic and professional aspirations. Wishing you continued success in your medical journey.
Pneumonia In Children And Adults

Introduction
Pneumonia stands as a prevalent respiratory infection, exerting a significant burden on global public health. Its impact extends beyond mere morbidity, contributing to substantial healthcare costs and socioeconomic consequences. This discussion aims to elucidate the general nature of pneumonia, encompassing its pathophysiology, clinical presentation, diagnostic modalities, treatment strategies, complications, and preventive measures. By indulging into these factors, we aim to provide a better understanding of pneumonia’s complexity and underscore the importance of timely recognition and management.
Pathophysiology

Pneumonia ensues from the infiltration of infectious agents, including bacteria, viruses, fungi, and less commonly, parasites, into the lower respiratory tract. Upon inhalation or aspiration of these pathogens, they gain access to the alveoli, where they incite an inflammatory response. This inflammatory cascade triggers the release of pro-inflammatory cytokines and chemokines, recruiting immune cells to the site of infection. Neutrophils, macrophages, and lymphocytes converge to eradicate the invading pathogens, leading to the characteristic consolidation and exudate formation within the affected lung tissue. As the infection progresses, alveolar edema, impaired gas exchange, and parenchymal damage ensue, culminating in the clinical manifestations of pneumonia.
Clinical Presentation

The clinical presentation of pneumonia encompasses a spectrum of symptoms, ranging from mild respiratory complaints to life-threatening respiratory failure. Common symptoms include cough, productive sputum production, fever, chills, pleuritic chest pain, dyspnea, tachypnea, and systemic manifestations such as malaise and fatigue. The severity of symptoms varies depending on factors such as the underlying pathogen, the extent of lung involvement, the host’s immune status, and comorbidities. In pediatric populations, pneumonia may present with nonspecific symptoms such as feeding difficulties, lethargy, and irritability, posing diagnostic challenges. Conversely, elderly individuals may exhibit atypical presentations characterized by confusion, hypothermia, and exacerbations of underlying chronic conditions.
Diagnostic Modalities

The diagnosis of pneumonia hinges on a comprehensive clinical assessment, augmented by various diagnostic modalities to confirm the presence of pulmonary infection and reveal its etiology. A thorough history and physical examination provide invaluable insights into the patient’s symptomatology, risk factors, and clinical trajectory. Symptomatic findings such as crackles, wheezes, and diminished breath sounds may aid in localizing the site of infection and assessing disease severity. Radiographic imaging, notably chest X-rays and computed tomography (CT) scans, serves as the cornerstone of pneumonia diagnosis, revealing characteristic radiographic findings such as airspace opacities, lobar consolidation, and interstitial infiltrates. Laboratory investigations, including complete blood count (CBC), C-reactive protein (CRP), and procalcitonin levels, may corroborate the clinical suspicion of pneumonia and guide therapeutic decisions. Additionally, microbiological testing of respiratory specimens through techniques such as sputum culture, blood cultures, and polymerase chain reaction (PCR) assays facilitates pathogen identification and antimicrobial susceptibility testing, thereby informing targeted therapy.
Treatment Strategies

The management of pneumonia hinges on prompt initiation of empiric antimicrobial therapy tailored to the likely causative pathogen(s) and disease severity. Antibiotics represent the mainstay of treatment for bacterial pneumonia, with the choice of agent dictated by factors such as local antimicrobial resistance patterns, patient age, comorbidities, and recent antibiotic exposure. Commonly prescribed antibiotics include beta-lactam agents (e.g., penicillins, cephalosporins), macrolides, fluoroquinolones, and combination regimens for severe or healthcare-associated infections. Conversely, viral pneumonia necessitates supportive care measures, given the limited efficacy of antiviral agents in most cases. Influenza-associated pneumonia may benefit from neuraminidase inhibitors such as oseltamivir, while respiratory syncytial virus (RSV) pneumonia may warrant ribavirin therapy in select cases. Adjunctive therapies such as oxygen supplementation, bronchodilators, and corticosteroids may mitigate respiratory distress and improve clinical outcomes, particularly in severe or hypoxemic patients. The duration of antimicrobial therapy varies depending on factors such as the causative pathogen, clinical response, radiographic resolution, and the presence of complications. Close monitoring of clinical parameters and serial imaging studies guide the decision-making process, enabling clinicians to tailor therapy to individual patient needs.
Complications

Pneumonia harbors the potential for various complications, ranging from mild to life-threatening sequelae, necessitating vigilant monitoring and timely intervention. Common complications include pleural effusion, empyema, lung abscess, respiratory failure, septic shock, and acute respiratory distress syndrome (ARDS). Pleural effusion denotes the accumulation of fluid within the pleural space, secondary to inflammation or impaired lymphatic drainage, manifesting as dyspnea, pleuritic chest pain, and dullness to percussion on physical examination. Empyema represents a purulent collection within the pleural cavity, often complicating bacterial pneumonia and necessitating drainage via thoracentesis or chest tube placement. Lung abscesses manifest as circumscribed cavities containing necrotic debris and pus within the lung parenchyma, triggered by persistent fever, productive cough, and hemoptysis. Respiratory failure ensues from impaired gas exchange and alveolar hypoventilation, caused by worsening hypoxemia, hypercapnia, and respiratory acidosis, necessitating mechanical ventilation and intensive care support. Septic shock represents a life-threatening complication of severe pneumonia, characterized by systemic inflammatory response syndrome (SIRS) and end-organ dysfunction, requiring aggressive fluid resuscitation, vasopressor therapy, and broad-spectrum antibiotics. ARDS denotes a severe form of acute lung injury, characterized by diffuse alveolar damage, refractory hypoxemia, and bilateral infiltrates on chest imaging, necessitating lung-protective ventilation and supportive care in the intensive care unit (ICU). The occurrence of complications portends a poor prognosis and underscores the need for early recognition and intervention to mitigate adverse outcomes.
Preventive Measures

Preventing pneumonia entails a broad approach encompassing vaccination, infection control measures, and health promotion strategies aimed at reducing the risk of respiratory infections and their sequelae. Vaccination stands as a cornerstone of pneumonia prevention, targeting common bacterial and viral pathogens implicated in pneumonia pathogenesis. Vaccines such as the pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) confer protection against Streptococcus pneumoniae, the leading bacterial cause of pneumonia, particularly in high-risk populations such as young children, older adults, and immunocompromised individuals. Influenza vaccination remains paramount in mitigating influenza-associated pneumonia and reducing disease transmission, underscoring the importance of annual vaccination campaigns targeting vulnerable populations. Additionally, adherence to infection control measures, including hand hygiene, respiratory etiquette, and environmental sanitation, plays a pivotal role in reducing the spread of respiratory pathogens in healthcare settings and the community at large. Health promotion efforts aimed at smoking cessation, optimizing nutrition, and addressing underlying comorbidities such as chronic obstructive pulmonary disease (COPD), asthma, and immunodeficiency bolster immune resilience and mitigate pneumonia risk. Furthermore, early identification and management of predisposing factors such as malnutrition, homelessness, and overcrowded living conditions attenuate pneumonia susceptibility and enhance overall health outcomes.
Conclusion
In conclusion, pneumonia emerges as a formidable respiratory infection, posing significant challenges to global public health. Its diverse etiology, clinical manifestations, diagnostic modalities, treatment modalities, complications, and preventive measures underscore the nature of pneumonia management. Timely recognition and intervention are imperative in mitigating the morbidity and mortality associated with pneumonia, necessitating a collaborative approach among healthcare providers, public health authorities, and policymakers. By fostering a comprehensive understanding of pneumonia’s manifest and implementing evidence-based strategies, we can strive towards reducing its burden and improving patient outcomes. Through ongoing research, education, and advocacy efforts, we can envision a future where pneumonia-related morbidity and mortality are substantially diminished, paving the way for enhanced respiratory health and well-being worldwide.
In managing pneumonia, compassion, empathy, and a holistic approach are essential alongside clinical expertise. Striving for excellence in knowledge and practice allows us to enhance respiratory medicine and patient outcomes.
As we address pneumonia and broader cardiovascular health complexities, let’s remain committed to optimal patient care. Together, we can impact lives positively and foster a healthier future.
Email expertassignment46@gmail.com to discover how we can support your academic and professional goals. Wishing you ongoing success in your medical journey.
Atherosclerosis

Introduction
Atherosclerosis is a chronic and progressive condition characterized by the accumulation of plaque within the walls of arteries, leading to their hardening and narrowing. Despite being often asymptomatic in its early stages, atherosclerosis poses significant risks to cardiovascular health and can result in severe complications such as heart attacks, strokes, and peripheral artery disease (PAD). Therefore, comprehensive knowledge of its symptoms, causes, prevention strategies, diagnosis methods, and treatment options is imperative for effectively managing its impact on individuals’ well-being.
Symptoms of Atherosclerosis

Atherosclerosis typically advances silently, with symptoms only becoming apparent as arteries become significantly obstructed or when a cardiovascular event occurs. The manifestation of symptoms varies depending on the affected arteries, each presenting distinct clinical presentations:
Coronary Arteries: The narrowing of coronary arteries due to atherosclerosis can lead to symptoms such as arrhythmia (irregular heartbeat), angina (chest pain or pressure), and shortness of breath, especially during physical exertion.
Cerebral Arteries: Atherosclerosis affecting cerebral arteries may manifest as numbness or weakness in the limbs, difficulty speaking or understanding speech, drooping facial muscles, paralysis, severe headache, or vision problems, indicating a heightened risk of stroke.
3. Peripheral Arteries: Individuals with atherosclerosis in peripheral arteries may experience symptoms such as leg pain when walking (intermittent claudication), numbness, cold extremities, aching or burning sensations in the feet, and slow-healing wounds or infections, reflecting compromised blood flow to the extremities
4. Renal Arteries: Atherosclerosis affecting renal arteries can result in elevated blood pressure (hypertension) and eventual kidney failure, highlighting the systemic impact of arterial narrowing on vital organ function.
Causes and Stages of Atherosclerosis

The development and progression of atherosclerosis involve a series of intricate biological processes initiated by damage to the endothelium, the delicate inner lining of arteries. As plaque composed of cholesterol, fat, calcium, and inflammatory substances accumulates within arterial walls, the disease progresses through distinct stages:
Damage to the Endothelium: The initial stage of atherosclerosis is characterized by injury to the endothelial cells lining the arteries, often attributed to risk factors such as high cholesterol, hypertension, inflammation, obesity, diabetes, and smoking.
2. Formation of Fatty Streaks: Following endothelial damage, the infiltration of low-density lipoprotein (LDL) cholesterol into the arterial wall triggers an inflammatory response, leading to the formation of fatty streaks — the earliest visible signs of atherosclerosis.
3 . Development of Fibrous Plaques: Over time, the accumulation of cholesterol-laden foam cells and the proliferation of smooth muscle cells contribute to the formation of fibrous plaques, which protrude into the arterial lumen and impede blood flow.
4 . Formation of Complicated Lesions: Advanced atherosclerosis is characterized by the formation of complicated lesions, where unstable plaques prone to rupture expose thrombogenic components, leading to the formation of blood clots and subsequent cardiovascular events such as myocardial infarction or ischemic stroke.
Risk Factors for Atherosclerosis
Numerous modifiable and non-modifiable risk factors influence the development and progression of atherosclerosis, underscoring the multifactorial nature of the disease. These risk factors include:
High Cholesterol: Elevated levels of LDL cholesterol, commonly referred to as “bad” cholesterol, promote the deposition of cholesterol within arterial walls, contributing to plaque formation and atherosclerosis progression.
2. High Blood Pressure: Hypertension exerts mechanical stress on arterial walls, accelerating endothelial damage and promoting atherosclerosis development
3. Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis or systemic lupus erythematosus, exacerbate endothelial dysfunction and foster plaque formation within arteries.
4. Obesity: Excess adiposity predisposes individuals to metabolic abnormalities, including dyslipidemia and insulin resistance, which fuel atherosclerosis progression.
5. Diabetes: Both type 1 and type 2 diabetes mellitus increase the risk of atherosclerosis by inducing endothelial dysfunction, promoting inflammation, and accelerating the formation of advanced glycation end-products (AGEs) implicated in vascular
6. Smoking: Tobacco smoke contains toxic compounds that promote endothelial injury, oxidative stress, and inflammation, exacerbating the progression of atherosclerosis and increasing the risk of cardiovascular events.
7.Sedentary Lifestyle: Physical inactivity contributes to metabolic derangements, including obesity, dyslipidemia, and insulin resistance, fostering atherosclerosis development and cardiovascular risk.
8. Family History of Heart Disease: Genetic predisposition plays a significant role in atherosclerosis susceptibility, with familial clustering of cardiovascular risk factors amplifying the likelihood of disease manifestation.
9. Poor Diet: Diets rich in saturated fats, trans fats, refined carbohydrates, and excess sodium promote dyslipidemia, hypertension, and endothelial dysfunction, fueling atherosclerosis progression.
9 .Stress: Chronic stress triggers sympathetic nervous system activation and cortisol release, contributing to hypertension, inflammation, and atherosclerosis development
10. Sleep Apnea: Obstructive sleep apnea, characterized by recurrent episodes of upper airway obstruction during sleep, disrupts normal cardiovascular function and exacerbates atherosclerosis progression.
Identifying and addressing these risk factors through targeted interventions and lifestyle modifications are essential for mitigating the burden of atherosclerosis and reducing the risk of cardiovascular events.
Diagnosis and Treatment of Atherosclerosis

Accurate diagnosis and effective management of atherosclerosis require a multidisciplinary approach involving clinical evaluation, imaging studies, and laboratory testing. Diagnostic modalities utilized in the assessment of atherosclerosis include:
Physical Examination: Healthcare providers perform a comprehensive physical examination, assessing vital signs, auscultating for abnormal heart sounds or bruits, and palpating for peripheral pulses to evaluate cardiovascular health.
Imaging Tests: Various imaging modalities are employed to visualize arterial anatomy, assess plaque burden, and identify areas of stenosis or occlusion. These includes;
Angiography: Intravascular contrast dye is utilized to visualize arterial lumens and detect areas of stenosis or occlusion via X-ray imaging.
Ultrasound: Non-invasive ultrasound techniques, such as carotid ultrasound or abdominal ultrasound, enable the assessment of arterial wall thickness, plaque morphology, and blood flow characteristics.
Computed Tomography (CT) Angiography: CT angiography provides detailed anatomical imaging of arterial structures, facilitating the identification of atherosclerotic lesions and assessing their severity.
Magnetic Resonance Angiography (MRA): MRA employs magnetic resonance imaging (MRI) techniques to generate high-resolution images of blood vessels, aiding in the evaluation of arterial stenosis, plaque composition, and hemodynamic parameters.
3. Laboratory Evaluations: Blood tests are conducted to assess lipid profiles, inflammatory markers, and other biochemical parameters associated with cardiovascular risk. These include
Lipid Profile: Measurement of serum lipid levels, including total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides, provides insight into atherosclerosis risk and treatment efficacy.
Inflammatory Markers: Assessment of inflammatory biomarkers, such as C-reactive protein (CRP) or interleukin-6 (IL-6), aids in risk stratification and monitoring disease activity in individuals with atherosclerosis.
Blood Glucose: Screening for abnormal glucose metabolism, including fasting blood glucose and hemoglobin A1c (HbA1c) levels, helps identify individuals at risk of diabetes-associated atherosclerosis complications
4. Functional Tests: Functional assessments, such as stress testing or ankle-brachial index (ABI) measurement, are performed to evaluate cardiovascular function and assess the impact of atherosclerosis on tissue perfusion.
Once diagnosed, the management of atherosclerosis encompasses various approach targeting risk factor modification, pharmacological intervention, and, when indicated, invasive procedures to alleviate arterial obstruction and prevent cardiovascular events.
Treatment strategies for atherosclerosis include:
Lifestyle Modifications: Lifestyle interventions form the cornerstone of atherosclerosis management, emphasizing dietary modifications, regular physical activity, smoking cessation, stress reduction, and weight management to optimize cardiovascular health and mitigate disease progression.
Medication Management: Pharmacological therapy plays a pivotal role in atherosclerosis treatment, targeting modifiable risk factors such as dyslipidemia, hypertension, and inflammation. Commonly prescribed medications include
Statins: HMG-CoA reductase inhibitors, such as atorvastatin or simvastatin, reduce LDL cholesterol levels and stabilize atherosclerotic plaques, lowering the risk of cardiovascular events.
Antihypertensive Agents: Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and calcium channel blockers are utilized to control blood pressure and mitigate endothelial dysfunction in individuals with hypertension-associated atherosclerosis.
Antiplatelet Therapy: Aspirin and other antiplatelet agents, such as clopidogrel or ticagrelor, inhibit platelet aggregation and reduce the risk of thrombotic events in individuals with established atherosclerosis or high cardiovascular risk.
Antidiabetic Medications: Oral hypoglycemic agents, insulin, or glucagon-like peptide-1 (GLP-1) receptor agonists are prescribed to achieve glycemic control and minimize the risk of diabetes-related atherosclerosis complications.
3. Invasive Procedures: In cases of severe arterial stenosis or symptomatic atherosclerotic disease refractory to medical therapy, invasive interventions may be warranted to restore arterial patency and alleviate ischemic symptoms. These include:
Percutaneous Coronary Intervention (PCI): Angioplasty with or without stent placement is performed to widen narrowed coronary arteries and improve myocardial perfusion in individuals with coronary artery disease (CAD).
Coronary Artery Bypass Grafting (CABG): Surgical revascularization using autologous or synthetic conduits bypasses obstructed coronary vessels, restoring blood flow to ischemic myocardial territories in patients with multivessel CAD or left main coronary artery disease.
Carotid Endarterectomy: Surgical removal of atherosclerotic plaque from carotid arteries reduces the risk of stroke in individuals with significant carotid stenosis and a history of transient ischemic attacks (TIAs) or cerebrovascular events.
Peripheral Arterial Interventions: Endovascular procedures, such as angioplasty, stenting, or atherectomy, are performed to treat lower extremity arterial disease and alleviate claudication symptoms in patients with peripheral artery disease (PAD).
Secondary Prevention Strategies: Beyond acute management, secondary prevention measures aim to prevent recurrent cardiovascular events and minimize disease progression through comprehensive risk factor modification, medication adherence, and ongoing surveillance of disease activity
Prevention of Atherosclerosis

Preventive strategies for atherosclerosis focus on addressing modifiable risk factors and promoting cardiovascular health through lifestyle modifications, health education, and targeted interventions. Key components of atherosclerosis prevention include:
Healthy Lifestyle: Encouraging individuals to adopt a healthy lifestyle characterized by balanced nutrition, regular physical activity, adequate sleep, stress management, and avoidance of harmful habits such as smoking or excessive alcohol consumption is paramount for reducing atherosclerosis risk
2. Dietary Modifications: Emphasizing a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and unsaturated fats while limiting intake of saturated fats, trans fats, cholesterol, sodium, and added sugars helps optimize lipid profiles, blood pressure, and overall cardiovascular health.
3. Physical Activity: Promoting regular exercise and physical activity is essential for maintaining cardiovascular fitness, weight management, insulin sensitivity, and endothelial function, thereby reducing the risk of atherosclerosis and its complications.
4. Tobacco Cessation: Implementing tobacco cessation programs and providing support for smoking cessation initiatives are critical for reducing atherosclerosis risk and improving overall cardiovascular outcomes.
5. Stress Management: Teaching stress reduction techniques such as mindfulness meditation, yoga, deep breathing exercises, or cognitive-behavioral therapy empowers individuals to cope with stressors effectively and mitigate their detrimental effects on cardiovascular health.
5 . Health Education: Educating individuals about the risks associated with atherosclerosis, the importance of early detection, and the benefits of preventive measures fosters informed decision-making and empowers individuals to take proactive steps towards cardiovascular wellness.
6. Regular Screening: Encouraging regular medical checkups and health screenings enables early detection of cardiovascular risk factors, facilitating timely intervention and personalized risk stratification for individuals at heightened risk of atherosclerosis.
Conclusion
In conclusion, atherosclerosis represents a significant public health challenge with far-reaching implications for cardiovascular morbidity and mortality. By majoring on the pathophysiology of atherosclerosis, identifying modifiable risk factors, and implementing evidence-based preventive strategies, healthcare providers can effectively mitigate the burden of atherosclerotic disease and promote cardiovascular health across diverse populations. Empowering individuals with knowledge, facilitating lifestyle modifications, and fostering a collaborative approach to atherosclerosis prevention and management are essential steps towards achieving optimal cardiovascular outcomes and enhancing quality of life for individuals affected by this pervasive condition.
As you navigate the complexities of cardiovascular health, remember that support and guidance are always available. Seek assistance from Expert Academic Assignment Help whenever needed.
Your journey in medicine is about more than just acquiring knowledge — it’s about embodying compassion, empathy, and continuous learning. Together, let’s strive for optimal cardiovascular health for all.
Email us at expertassignment46@gmail.com
Wishing you success and fulfillment in your medical journey.
Cerebral Palsy

Introduction
Cerebral palsy (CP) is not only a neurological condition but also a lifelong journey for individuals and their families. The impacts of CP extend far beyond physical limitations, encompassing social, emotional, and economic aspects. Understanding the complexities of CP is crucial for healthcare professionals, educators, policymakers, and society at large to provide adequate support and resources for affected individuals.
In recent years, there has been a growing recognition of the diversity within the CP community, with an emphasis on individualized care and inclusive practices. By fostering a deeper understanding of CP, we can promote empowerment, advocacy, and meaningful participation for individuals with CP in all aspects of life.
Symptoms and Types

The symptoms of CP can manifest in various ways, depending on the severity and type of the condition. For some individuals, muscle stiffness or spasticity may be the predominant feature, leading to difficulties in movement and coordination. Others may experience involuntary movements or dyskinetic movements, characterized by writhing or twisting motions. Mixed types of CP present with a combination of spastic and dyskinetic features, further complicating the clinical picture.
In addition to motor impairments, individuals with CP may also experience associated conditions such as intellectual disability, epilepsy, communication difficulties, and sensory impairments. These coexisting conditions can significantly impact the daily lives of affected individuals and require comprehensive management strategies tailored to their unique needs.
Causes and Risk Factors

Prenatal factors such as premature birth, low birth weight, maternal infections, and genetic abnormalities play a significant role in the development of CP. Maternal health conditions like preeclampsia and gestational diabetes may also increase the risk of CP, highlighting the importance of maternal health during pregnancy.
Perinatal events such as birth asphyxia, neonatal stroke, or brain hemorrhage can result in brain injury and subsequent CP. Postnatal factors such as traumatic brain injury, infections, or accidents can also contribute to the development of CP, underscoring the need for vigilance and prompt intervention in the neonatal period and beyond.
Certain maternal and environmental factors, including multiple pregnancies, maternal substance use, and advanced maternal age, may further predispose individuals to CP. Addressing these modifiable risk factors through public health initiatives, prenatal care, and early intervention programs is essential for reducing the burden of CP on affected individuals and their families.
Diagnosis and Management

The diagnosis of CP is often made based on clinical assessment and observation of motor impairments, developmental delays, and associated conditions. Medical history, including prenatal, perinatal, and postnatal factors, provides valuable insights into potential risk factors and contributing factors for CP. Developmental assessments, such as the Denver Developmental Screening Test or the Bayley Scales of Infant and Toddler Development, can help identify delays in reaching developmental milestones and guide early intervention strategies.
Physical examination plays a critical role in evaluating muscle tone, reflexes, coordination, and posture. Neuroimaging studies, including magnetic resonance imaging (MRI) and computed tomography (CT) scans, may reveal structural abnormalities or lesions in the brain indicative of CP. These diagnostic tools help healthcare professionals confirm the diagnosis of CP and tailor management strategies to address the specific needs of affected individuals.
Early intervention is paramount in optimizing outcomes for individuals with CP, as neuroplasticity is greatest during the early years of life. A multidisciplinary approach involving healthcare professionals from various disciplines, including pediatricians, neurologists, physiatrists, physical therapists, occupational therapists, speech therapists, and social workers, ensures comprehensive care and support for affected individuals and their families.
Management strategies for CP encompass a range of interventions aimed at addressing motor impairments, enhancing functional abilities, and promoting independence. Medical interventions may include medications to manage symptoms such as spasticity, seizures, or associated conditions. Physical therapy focuses on improving mobility, strength, and coordination through exercises, stretches, and functional activities. Occupational therapy helps individuals develop skills for activities of daily living, such as feeding, dressing, and grooming. Speech therapy addresses communication difficulties and swallowing disorders, enhancing oral motor skills and facilitating effective communication. Orthotic devices, such as braces or splints, may be prescribed to improve posture, stability, and mobility. Assistive technology, including communication devices, mobility aids, and adaptive equipment, can enhance independence and quality of life for individuals with CP. Surgical interventions, such as selective dorsal rhizotomy or orthopedic procedures, may be considered to reduce spasticity, correct musculoskeletal deformities, or improve functional outcomes.
The management of CP is highly individualized, with treatment plans tailored to address the specific needs and goals of each individual. Regular follow-up visits with healthcare providers allow for ongoing assessment, monitoring, and adjustment of management strategies as needed. Family-centered care, collaboration between healthcare professionals, educators, and community resources, and advocacy for inclusive practices are essential in supporting individuals with CP and promoting their overall well-being.
Prognosis and Living With CP

The prognosis for individuals with CP varies widely depending on various factors, including the severity and type of CP, the presence of associated conditions, access to medical care and supportive services, and individual factors such as resilience, motivation, and social support. While some individuals may experience significant functional limitations and require lifelong assistance, others may achieve remarkable milestones and lead independent lives.
Advances in medical care, including early intervention programs, multidisciplinary care teams, and innovative treatment modalities, have contributed to improved outcomes and quality of life for individuals with CP. Early identification and intervention, coupled with ongoing support and rehabilitation services, play a crucial role in optimizing functional outcomes and promoting independence.
Living with CP requires resilience, perseverance, and adaptation to overcome physical, emotional, and social challenges. Individuals with CP may face barriers to participation in education, employment, and social activities due to mobility limitations, communication difficulties, and societal attitudes toward disability. Advocacy efforts, disability rights initiatives, and inclusive policies are essential in promoting equal opportunities, accessibility, and social inclusion for individuals with CP.
Family support, peer networks, and community resources play a vital role in providing emotional support, practical assistance, and social connections for individuals with CP and their families. Building resilience, fostering independence, and nurturing self-esteem are essential in empowering individuals with CP to advocate for their needs, pursue their goals, and lead fulfilling lives.
Conclusion
Cerebral palsy is a complex neurological disorder that requires a comprehensive understanding and multidisciplinary approach to diagnosis, management, and support. By addressing the diverse needs of affected individuals and their families, fostering inclusive practices, and advocating for equal opportunities, we can promote the well-being and full participation of individuals with CP in society. Continued research, education, and advocacy are essential in advancing our understanding of CP, improving outcomes, and enhancing the quality of life for affected individuals and their families
Remember, success in your academic endeavors is within reach. Whether you’re facing challenges or seeking to elevate your performance, don’t hesitate to reach out for expert guidance and support. I’m here to assist you every step of the way. Reach me at williamsassignmenthelpfredrick@gmail.com
Let’s embark on this journey towards academic excellence together. Looking forward to hearing from you soon.
Your Digestive System & How it Works

Introduction
The digestive system is a marvel of biological process that involves the breakdown of food into absorbable nutrients essential for sustaining life. Comprising a network of organs and tissues, it serves as the body’s processing center, converting ingested substances into energy, growth materials, and waste. Understanding the intricacies of this system provides profound insights into human physiology and health maintenance.
1. Anatomy of the Digestive System

The digestive system is a complex network of organs, glands, and tissues that work in harmony to facilitate the digestion and absorption of nutrients. At its core lies the gastrointestinal tract (GI tract), a continuous tube extending from the mouth to the anus. Key components of the GI tract include the mouth, esophagus, stomach, small intestine, large intestine, and anus. Additionally, accessory organs such as the liver, pancreas, and gallbladder contribute crucial digestive enzymes and fluids to aid in the breakdown of food.
2. Functions of the Digestive System

The primary function of the digestive system is to process food and liquids to extract essential nutrients while eliminating waste products. Through a series of coordinated processes, including ingestion, digestion, absorption, and excretion, the digestive system ensures the body receives the necessary components for energy production, tissue repair, and growth. Moreover, it plays a vital role in maintaining fluid and electrolyte balance within the body.
3. Digestive process

Digestion begins in the mouth, where mechanical and chemical processes break down food into smaller particles. Chewing, or mastication, mechanically reduces food size, while saliva, secreted by salivary glands, initiates the chemical breakdown of carbohydrates through the action of enzymes like amylase. The bolus of food then travels down the esophagus via peristaltic contractions, entering the stomach for further processing.
In the stomach, gastric juices containing hydrochloric acid and pepsin begin the breakdown of proteins, while muscular contractions churn the food into a semi-liquid mixture known as chyme. From the stomach, chyme enters the small intestine, where the majority of nutrient absorption occurs. Enzymes from the pancreas and bile from the liver aid in the breakdown of fats, proteins, and carbohydrates, allowing for absorption across the intestinal lining.
In the large intestine, water absorption occurs, leading to the formation of feces. Microbial fermentation within the colon further breaks down indigestible carbohydrates and produces essential nutrients like vitamin K and certain B vitamins. Finally, waste products are expelled through the anus during defecation.
4. Regulation of Digestive Processes

The intricate processes of digestion are tightly regulated by a combination of neural, hormonal, and local mechanisms. Neural signals originating from the brain and enteric nervous system (ENS) coordinate muscle contractions along the GI tract, ensuring the smooth passage of food and efficient mixing with digestive juices. Hormones such as gastrin, secretin, and cholecystokinin act as chemical messengers, modulating gastric acid secretion, pancreatic enzyme release, and bile production in response to dietary stimuli.
5. Clinical Implications and Disorders

Disruptions to the normal functioning of the digestive system can lead to a myriad of health disorders, ranging from minor discomforts to life-threatening conditions. Gastrointestinal disorders encompass a broad spectrum of diseases, including gastroesophageal reflux disease (GERD), peptic ulcers, inflammatory bowel disease (IBD), and colorectal cancer. These conditions often manifest with symptoms such as abdominal pain, bloating, diarrhea, constipation, and rectal bleeding, necessitating thorough diagnostic evaluation and tailored treatment approaches.
6. Research and Advancements

Advancements in medical research continue to deepen our understanding of digestive physiology and pathology, paving the way for innovative diagnostic techniques and therapeutic interventions. Clinical trials conducted by academic institutions and pharmaceutical companies play a pivotal role in evaluating novel treatment modalities and improving patient outcomes. Areas of active investigation include microbiome research, targeted drug delivery systems, and minimally invasive surgical techniques for gastrointestinal disorders.
Conclusion
In conclusion, the digestive system serves as a cornerstone of human biology, enabling the breakdown and assimilation of nutrients essential for life. Its intricate anatomy and physiological processes underscore the remarkable complexity of the human body. By elucidating the mechanisms of digestion and exploring the clinical implications of digestive disorders, we gain valuable insights into the maintenance of health and the management of disease. Continued research efforts hold the promise of further enhancing our understanding and treatment of gastrointestinal conditions, ultimately improving the quality of life for individuals worldwide.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
Brain Tumor

Introduction
Brain tumors represent a complex and diverse group of neoplasms that arise from abnormal growth of cells within the brain or its surrounding structures. These tumors can vary widely in terms of their location, size, aggressiveness, and clinical presentation. Understanding the intricacies of brain tumors, including their diagnosis, treatment, and prognosis, requires a comprehensive approach that integrates medical expertise, advanced imaging modalities, and personalized therapeutic interventions.
Diagnosis of Brain Tumor

The diagnosis of a brain tumor typically begins with a thorough clinical evaluation, including a detailed medical history and neurological examination. Symptoms suggestive of a brain tumor may include persistent headaches, seizures, cognitive deficits, changes in behavior or personality, and focal neurological deficits such as weakness or sensory disturbances. However, it’s essential to recognize that many of these symptoms are nonspecific and can be caused by various other conditions.
To confirm the presence of a brain tumor and characterize its specific features, a variety of imaging studies and laboratory tests may be employed. These include computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans. CT scans provide detailed cross-sectional images of the brain and are often the initial imaging modality used to assess patients with suspected brain tumors due to their widespread availability and rapid results. MRI, on the other hand, offers superior soft tissue contrast and is particularly useful for delineating the precise location and extent of brain tumors. In some cases, contrast-enhanced MRI with gadolinium-based contrast agents may be performed to enhance visualization of tumor tissue and surrounding structures.
Advanced MRI techniques, such as functional MRI (fMRI), magnetic resonance spectroscopy (MRS), and perfusion-weighted imaging (PWI), can provide additional information about the functional characteristics and metabolic activity of brain tumors. These modalities play a crucial role in treatment planning and assessing tumor response to therapy.
In select cases, a PET scan may be utilized to evaluate the metabolic activity of brain tumors and differentiate between benign and malignant lesions. PET imaging with radiopharmaceutical tracers such as fluorodeoxyglucose (FDG) can help identify areas of increased glucose metabolism, which are typically indicative of rapidly growing tumor cells. Additionally, molecular imaging techniques targeting specific biomarkers may offer insights into the molecular profile and biological behavior of brain tumors, facilitating personalized treatment strategies.
Tissue Sampling and Histopathological Evaluation: While imaging studies provide valuable information about the radiographic characteristics of brain tumors, definitive diagnosis often requires histopathological analysis of tissue samples obtained via biopsy or surgical resection. Tissue sampling allows for detailed microscopic examination of tumor cells, assessment of histological features, and determination of tumor grade, which plays a crucial role in prognostication and treatment planning.
Brain tumor grading is based on the World Health Organization (WHO) classification system, which stratifies tumors into different grades (I-IV) based on their histological features and biological behavior. Grade I tumors are typically slow-growing and well-differentiated, while grade IV tumors are highly aggressive and rapidly proliferating. Intermediate grades (II-III) exhibit varying degrees of aggressiveness and cellular atypia.
Prognostic Factors and Treatment Consideration

The prognosis of patients with brain tumors is influenced by various factors, including tumor type, grade, location, extent of resection, molecular characteristics, and patient-specific factors such as age and overall health status. High-grade tumors, such as glioblastoma multiforme, are associated with poorer outcomes compared to low-grade tumors, necessitating more aggressive treatment approaches.
Treatment strategies for brain tumors are highly individualized and may encompass a combination of surgical resection, radiation therapy, chemotherapy, targeted therapy, and supportive care measures. The goals of treatment are to achieve maximal tumor control while preserving neurological function and quality of life. Surgical resection is often the initial step in the management of operable brain tumors, with the aim of achieving gross total resection whenever feasible. However, the proximity of tumors to critical brain structures and eloquent areas may limit the extent of surgical resection and necessitate adjuvant therapies.
Surgical Management of Brain Tumor

Surgical approaches to brain tumor resection have evolved significantly with advances in neuroimaging, neurosurgical techniques, and intraoperative navigation systems. Traditional open craniotomy remains the standard approach for many brain tumors, allowing for direct access to the intracranial lesion. Microsurgical techniques, including the use of operating microscopes and intraoperative neuro navigation systems, enable precise tumor localization and maximal safe resection while minimizing damage to adjacent healthy brain tissue.
In recent years, minimally invasive approaches such as endoscopic endonasal surgery and keyhole craniotomy have gained popularity for select brain tumors, offering advantages such as smaller incisions, reduced surgical morbidity, and faster recovery times. Endoscopic techniques, in particular, allow for access to deep-seated lesions through natural orifices, such as the nasal cavity, thereby avoiding the need for extensive craniotomies and brain retraction.
Radiation Therapy for Brain Tumors

Radiation therapy plays a critical role in the management of both primary and metastatic brain tumors, offering precise and localized delivery of ionizing radiation to target tumor cells while sparing adjacent normal brain tissue. External beam radiation therapy (EBRT) is the most commonly utilized modality, utilizing high-energy X-rays or protons to deliver radiation to the tumor site over multiple treatment sessions. Techniques such as intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery (SRS) allow for highly conformal dose delivery, enabling escalation of radiation doses to the tumor while minimizing toxicity to surrounding critical structures.
In addition to conventional EBRT, brachytherapy techniques may be employed for selected cases, involving the placement of radioactive sources directly into or adjacent to the tumor cavity during surgical resection. This allows for localized delivery of high-dose radiation while minimizing exposure to healthy tissues. Proton therapy, a form of particle therapy, offers the advantage of improved dose conformity and reduced integral dose to surrounding tissues compared to conventional photon-based radiation therapy. Proton therapy is particularly beneficial for treating pediatric brain tumors and tumors located near critical structures, such as the optic nerves and brainstem.
Chemotherapy and Targeted Therapy: Chemotherapy plays a crucial role in the management of certain brain tumors, particularly high-grade gliomas and metastatic lesions. Chemotherapeutic agents may be administered orally, intravenously, or intracranially, either as monotherapy or in combination with other treatment modalities. The choice of chemotherapy regimen depends on factors such as tumor type, molecular characteristics, and patient-specific considerations.
Targeted therapy has emerged as a promising treatment approach for select brain tumors, leveraging the identification of specific molecular targets or pathways implicated in tumor growth and progression. Targeted agents may include small molecule inhibitors, monoclonal antibodies, or immunotherapeutic agents designed to selectively target tumor cells while sparing normal tissues. Biomarker-driven approaches, such as molecular profiling and genetic testing, help identify patients who are most likely to benefit from targeted therapies, enabling a personalized approach to treatment selection.
Recovery and Rehabilitation

Recovery following treatment for brain tumors often requires comprehensive rehabilitation efforts aimed at optimizing functional outcomes and quality of life. Physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation play important roles in addressing deficits related to motor function, activities of daily living, communication, and cognition. Additionally, psychosocial support services and caregiver education are essential components of the multidisciplinary care team, providing emotional support and practical assistance to patients and their families throughout the treatment and recovery process.
Conclusion
In conclusion, the management of brain tumors necessitates a multidisciplinary and individualized approach that integrates advances in diagnostic imaging, surgical techniques, radiation therapy, chemotherapy, targeted therapy, and supportive care interventions. Collaborative decision-making between patients, healthcare providers, and allied health professionals is paramount in optimizing treatment outcomes and enhancing quality of life for individuals affected by brain tumors. Ongoing research efforts aimed at elucidating the molecular mechanisms underlying tumorigenesis, identifying novel therapeutic targets, and refining treatment strategies offer hope for continued advancements in the field of neuro-oncology and improved outcomes for patients with brain tumors.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
10 Common Dental Problems

Introduction
Maintaining optimal dental health is crucial not only for a winning smile but also for overall well-being. However, numerous individuals encounter common dental issues that can affect their quality of life. From tooth decay to gum disease, understanding these problems and their treatments is essential for preventing complications and preserving oral health. This comprehensive guide explores ten prevalent dental problems and outlines effective treatment options for each, empowering individuals to make informed decisions about their dental care.
1.Tooth Decay

Tooth decay, also known as dental caries, is a pervasive dental issue caused by the accumulation of plaque and the subsequent erosion of tooth enamel. This section delves into the causes, symptoms, and treatment options for tooth decay, emphasizing the importance of preventive measures such as regular brushing, flossing, and dental check-ups.
2. Gum Disease

Gingivitis and periodontitis are two stages of gum disease characterized by inflammation and bacterial infection of the gums. Exploring the risk factors, symptoms, and management strategies for gum disease sheds light on the importance of proper oral hygiene practices and professional dental interventions in preserving gum health.
3.Bad Breath

Halitosis, or bad breath, can stem from various underlying factors such as poor oral hygiene, dry mouth, and underlying medical conditions. This segment examines the causes of bad breath and highlights the significance of comprehensive dental assessments and tailored treatment plans to address this common concern effectively.
4.Sensitive Teeth

Tooth sensitivity, characterized by discomfort in response to hot, cold, or sweet stimuli, often results from enamel erosion or underlying dental issues. Delving into the potential causes and management options for sensitive teeth underscores the role of personalized dental care in alleviating discomfort and enhancing oral comfort.
5.Cracked or Broken Teeth

Cracks or fractures in teeth can result from trauma, bruxism (teeth grinding), or other factors, leading to pain and functional impairment. This section explores the diagnostic procedures and treatment modalities available for repairing cracked or broken teeth, emphasizing the importance of prompt intervention to prevent further damage.
6.Receding Gums

Receding gums, characterized by the exposure of tooth roots due to gum tissue loss, can result from various factors, including poor oral hygiene and genetic predispositions. Analyzing the causes, consequences, and treatment approaches for receding gums underscores the significance of preventive measures and professional interventions in preserving gum health.
7. Root Infection

Root infections, often resulting from untreated cavities or trauma, can lead to severe pain and dental abscesses if left untreated. This segment elucidates the diagnostic techniques and treatment options for root infections, highlighting the role of root canal therapy in alleviating symptoms and preserving tooth structure.
8. Enamel Erosion

Enamel erosion, characterized by the gradual loss of tooth enamel due to acidic and sugary dietary habits, poses significant challenges to dental health. Exploring preventive strategies and restorative treatments for enamel erosion underscores the importance of dietary modifications and proactive dental care in preserving tooth structure and function.
9. Dry Mouth

Xerostomia, or dry mouth, can result from various factors, including medication side effects and underlying medical conditions. This section examines the causes, symptoms, and management strategies for dry mouth, emphasizing the importance of hydration and lifestyle modifications in alleviating discomfort and preventing oral complications.
10. Teeth Grinding
Bruxism, characterized by involuntary teeth grinding or clenching, can lead to tooth wear, jaw pain, and headaches. Exploring the underlying causes and treatment options for bruxism underscores the importance of stress management and protective dental appliances in mitigating symptoms and preserving dental health.
Conclusion
In conclusion, understanding and addressing common dental problems are essential steps toward maintaining optimal oral health and overall well-being. By recognizing the signs and symptoms of tooth decay, gum disease, and other dental issues, individuals can seek timely intervention and preventive care to mitigate risks and preserve their smiles. Through a combination of proper oral hygiene practices, regular dental check-ups, and personalized treatment plans, individuals can navigate common dental challenges with confidence and achieve lasting oral health. Embracing proactive dental care and seeking professional assistance when needed are crucial components of a comprehensive approach to dental wellness.
In exploring and pursuing your dental studies, we wish you all the best in becoming a dentist. In case you encounter challenges or need guidance during this study period, do not hesitate to contact us.
Email at;williamsassignmenthelpfredrick@gmail.com
Breast Cancer

Introduction
Breast cancer, a multifaceted and prevalent disease, poses a significant health challenge globally, transcending gender lines with its potential impact. Characterized by the abnormal proliferation of cells within breast tissue, breast cancer’s complex etiology remains an area of intense study and concern. Despite notable advancements in medical science and increased awareness, it continues to be a leading cause of morbidity and mortality worldwide. This comprehensive discussion aims to delve into the intricacies of breast cancer, encompassing its causes, risk factors, prevention strategies, diagnostic modalities, treatment options, and the evolving landscape of supportive care.
Causes and Risk Factors

Understanding the underlying causes and risk factors associated with breast cancer is paramount in developing effective prevention and management strategies. While the precise etiology of breast cancer remains elusive, various genetic, hormonal, environmental, and lifestyle factors contribute to its onset and progression. Genetic predispositions, such as mutations in the BRCA1 and BRCA2 genes, significantly elevate the risk of developing breast cancer. Additionally, hormonal influences, including early onset of menstruation, late menopause, and hormone replacement therapy, play a crucial role in disease pathogenesis. Lifestyle factors such as excessive alcohol consumption, obesity, lack of physical activity, and exposure to environmental carcinogens further augment the risk profile.
Preventive Measures

Empowering individuals with knowledge about preventive measures is essential in mitigating the burden of breast cancer. Promoting regular breast self-examinations, clinical breast examinations, and mammographic screenings facilitates early detection and intervention. Emphasizing lifestyle modifications, including maintaining a healthy weight, adopting a balanced diet rich in fruits and vegetables, limiting alcohol intake, and engaging in regular physical activity, can reduce the risk of breast cancer. For individuals with a heightened risk due to genetic predispositions or familial history, prophylactic surgeries, such as mastectomy or oophorectomy, and chemo preventive agents offer viable preventive options.
Diagnostic Modalities

Advances in diagnostic modalities have revolutionized the early detection and diagnosis of breast cancer, enabling prompt initiation of treatment and improved clinical outcomes. Mammography remains the cornerstone of breast cancer screening, capable of detecting abnormalities such as microcalcifications, masses, or architectural distortions. Complementary imaging techniques, including ultrasound, magnetic resonance imaging (MRI), and molecular breast imaging (MBI), enhance diagnostic accuracy, particularly in women with dense breast tissue or high-risk profiles. Biopsy procedures, such as core needle biopsy or surgical excision, facilitate histopathological examination, enabling precise diagnosis and classification of breast lesions.
Treatment Options

Tailoring treatment strategies to individual patient characteristics and disease parameters is essential in optimizing therapeutic outcomes in breast cancer. The treatment landscape encompasses a multidisciplinary approach, integrating surgical, medical, and radiation oncology interventions. Surgical options range from breast-conserving surgeries, such as lumpectomy or segmental mastectomy, to radical procedures like total mastectomy or modified radical mastectomy, depending on tumor size, location, and extent of spread. Adjuvant therapies, including chemotherapy, hormonal therapy, targeted therapy, and immunotherapy, aim to eradicate residual disease, prevent recurrence, and improve overall survival. Radiation therapy, administered either postoperatively or as a primary modality in selected cases, targets residual tumor cells, minimizing locoregional recurrence rates.
Supportive Care and Survivorship

Recognizing the holistic needs of breast cancer patients and survivors is integral in promoting comprehensive care and ensuring optimal quality of life. Supportive care interventions, including symptom management, psychosocial support, nutritional counseling, and rehabilitation services, address the multifaceted challenges associated with cancer diagnosis and treatment. Survivorship programs, focusing on survivorship care planning, surveillance for recurrence, long-term monitoring of treatment-related complications, and health promotion initiatives, facilitate the transition from active treatment to survivorship. Engaging patients and caregivers in survivorship care planning fosters empowerment, resilience, and a sense of agency in navigating the post-treatment phase.
Conclusion
In conclusion, breast cancer represents a formidable health challenge with profound implications for affected individuals, families, and communities worldwide. While significant strides have been made in understanding its pathophysiology, enhancing diagnostic capabilities, and expanding treatment options, concerted efforts are warranted to address existing gaps in prevention, early detection, and access to care. By fostering collaborative partnerships among stakeholders, advocating for evidence-based interventions, and promoting health equity, we can strive towards a future where breast cancer incidence and mortality rates are substantially reduced. Through continued innovation, education, and advocacy, we can transform the landscape of breast cancer care, offering hope, support, and healing to those impacted by this pervasive disease.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com